Tuberculosis:
Pulmonary tuberculosis (TB) is a chronic infectious disease caused by Mycobacterium tuberculosis that primarily affects lung parenchyma. Tuberculosis is curable and preventable.
TB is the top 10 causes of death and the leading cause from a single infectious agent (above HIV/AIDS)
Many strains of tuberculosis resist the drugs most used to treat the disease. People with active tuberculosis must take several types of medications for many months to eradicate the infection and prevent the development of antibiotic resistance.
Causative agent
- Mycobacterium tuberculosis (also known as tubercle bacilli) less likely M.Bovi and M.africanum
- Acid-fast bacilli
- Remain dormant tissue and persist for many years
Risk factor
- Elderly and infant
- Low socioeconomic status
- Immunodeficiency like HIV/AIDS
- Alcoholism, smoking
1.1 million children (0–14 years of age) fell ill with TB, and 230 000 children (including children with HIV associated TB) died from the disease in 2018.
Alcohol use disorder and tobacco smoking increase the risk of TB disease by a factor of 3.3 and 1.6, respectively. In 2018, 0.83 million new TB cases worldwide were attributable to alcohol use disorder and 0.86 million were attributable to smoking.
Transmission
- Caused by breathing air droplet from cough or sneeze of an infected person
- one cough can produce 3000 droplet nuclei
- Sunlight and ventilation reduces the risk of transmission
When a person develops active TB disease, the symptoms (such as cough, fever, night sweats, or weight loss) may be mild for many months. This can lead to delays in seeking care, and results in the transmission of the bacteria to others. A person needs to inhale only a few of these germs to become infected.
Natural history of the disease
- 90% of people who are infected with tubercle bacilli do not develop active disease
- Can be diagnosed with positive tuberculin skin test
- Without treatment, after 5 years 50%of patient died, 25% will be healthy and 25% will remain ill with chronic infectious disease
Types of Pulmonary Tuberculosis
- primary PTB
- progressive PTB
- post-primary or secondary PTB
Primary PTB: Primary Pulmonary Tuberculosis describes the pulmonary pathology and clinical consequences that result following initial infection with M. tuberculosis.
- Exposure to bacilli
- Droplet nuclei lodge in alveoli
- Ingested by alveolar macrophage
- Multiplication of tubercle bacilli in the lungs (ghons focus)
- Lymphatic drain the bacilli to the hilar lymph nodes
- primary complex-ghons focus and related hilar lymphadenopathy
Outcome of primary PTB :
- No clinical disease positive tuberculin skin test (usual outcome in over 90%of cases
- Hypersensitivity reactions: Erythema nodusom phyctenullar conjunctivitis
- Pulmonary and pleural complication
- Tubercular pneumonia
- Lobar collapse (bronchial compression )
- Pleural effusion
- Disseminated disease:
- Lymphadenopathy (usually cervical)
- meningitis
- Pericarditis
- Milliary disease
Secondary PTB: Reactivation of the latent infection and is usually localized to the apical and posterior segment of upper lobe.
Secondary tuberculosis is usually due to the reactivation of old lesions or gradual progression of primary tuberculosis into a chronic form. However, recent evidence suggests that reinfection is responsible for some of secondary tuberculosis. The characteristics of secondary tuberculosis include extensive tissue damages due to the immunologic reactions of the host to tubercle bacilli and their products.
Symptoms
constitutional symptoms
- Fatigue
- fever/night sweats
- Unintentional weight loss
- loss of appetite
Respiratory symptoms
- Chest pain
- Wheezing
- Breathing difficulty
- Haemoptysis
- cough with sputum production
Investigations
- Blood – CBC,ESR ,CRP
- Sputum: stain
- 3 sputum samples
- Early morning sample is preferred
- Ziehl-Neelsen stain
- culture
Note: if any two of the sputum sample is positive then PTB is diagnosed
- Tuberculin skin test(Mantoux test):
- tuberculin purified protein 0.5ml derived from tubercle bacteria is injected into the dermis
- Delayed hypersensitivity reaction after 24-48 hour
- positive case if induration diameter >10mm -infection
- Consider positive if >5 mm immunocompromised
- does not distinguish between active and latent infection
LABORATORY FINDINGS:
- Mantoux test
Injecting a small amount of protein from tuberculosis bacteria between the layer of skin
- Sputum examination and culture
IMAGING:
- Chest X-ray:
No chest X-ray pattern is typical of PTB
Classical pattern
-
- Upper lobe infiltration
- Bacterial infiltration
- Cavitation
- Pulmonary fibrosis and shrinkage
- Pleural effusion
- Miliary pattern
- Chest CT scan
- Per amplification
COMPLICATIONS:
- Bones
- Brain (meningitis )
- Heart(cardiac tamponade)
- Pleural effusion
- Serious reaction to drug therapy(hepatotoxicity and hypersensitivity)
ALSO READ :
Pneumonia Classification, Causes, Pathophysiology, Management and Prevention
Treatment of Pulmonary TB
- Pulmonary TB: Treat with the antitubercular agent for 6 -12 month
- Isoniazid (H) – bactericidal 5 mg/kg/day
- Rifampicin – bactericidal 10 mg/kg/day
- Pyrizinamide – bactericidal 25 mg/kg /day
- Ethambutol – bacteriostatic 15 mg/kg day
- Streptomycin-bactericidal 15 mg/kg/day
Treatment Category
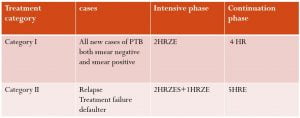
Case definition:
- New case
- Never had treatment of TB or
- has taken the antituberculosis drug for less than 4 week
- Relapse
- Who has been cured and completed treatment, but again has sputum smear-positive TB
- Treatment failure
- Who remains become sputum smear-positive for 5 months or more after starting treatment
- Defaulter
- A registered patient who missed more than 60 days of anti-tuberculosis treatment and starting treatment for TB again
DOTS (Directly observed treatment short course): WHO-recommended TB treatment strategy
- Case detection by sputum smear microscope
- Stander treatment regimen directly observed by a health worker or community health worker for at least the first 2 months
- A regular drug supply standardized recording and reporting system for assessment of the result
Indication for steroid
- TB meningitis
- TB pericarditis
- TB pleural effusion (symptomatic)
- TB of the adrenal gland
- TB laryngitis
- Severe hypersensitivity reaction to anti TB drug
- renal tract TB
- Massive lymph node enlargement with pressure effects
Reference: WHO