Definition:
Asthma is a chronic inflammatory disorder of the airway that is characterized by
- Clinically by recurrent episodes of wheezing breathless chest tightness and cough particularly at night or early morning
- physiologically by widespread reversible narrowing of the bronchial airways and a marked increase in bronchial responsiveness

According to CDC more than 25 million Americans, including 6.8 million children under age 18 suffer from asthma
Asthma is associated with mast cell eosinophils and lymphocytes mast cell are the allergy-causing cell that releases chemical like histamine is the substance that causes nasal stiffness and dripping in the cold and hay fever constriction of airways in asthma and itchy area in the skin allergy eosinophils are the type of white blood cell-associated with allergy disease T lymphocytes are also white blood cell associated with allergy and inflammation.
Classification :
- Atopic /extrinsic /allergic (70%)
- IgE mediated immune response to environmental antigens
- Non-atopic /intrinsic /non-allergic
- Triggered by non-immune stimuli patient have a negative skin test to common inhaled allergens and normal serum contraction of IgEasthma may be triggered by aspirin pulmonary infection, cold stress, or inhaled irritants
Precipitating factor
- Allergens
- Cold air
- Virus infection
- Drug
- Exercise
- Food
- Air pollutants
- Physical factor
- Stress
- Occupational factor
- GERD (gastroesophageal reflux disordered )
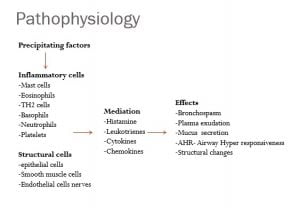
Pathophysiology of Bronchial Asthma
Precipitating factor
↓
inflammatory cell
- Mast cell
- Eosinophils
- TH2 cell
- Basophils MEDIATION EFFECTS
- Neutrophils → Histamine → Bronchospasm
- Platelets Lukotriness Plasma exudations
Cytokines Mucus secretion
Chemokines AHR- Airway hyperresponsiveness
Structural Changes
Structural cell
- Epithelial cell
- Smooth muscle cell
- Endothelial cell nerve
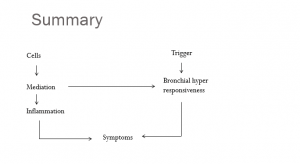
Summary of Pathophysiology of Bronchial Asthma
Clinical presentation :
- Wheezing, dyspnea, and cough (variable – both spontaneously and with therapy
- Sputum worse at night or early morning
- Limitation of activity
- Mucoid Sputum
Sign:
- Increase respiratory rate with the use of accessory muscle
- Hyper resonant percussion note
- Expiratory wheeze, expiration, is longer than Inspiration
- During very severe attacks airflow may be insufficient to produce wheeze (silent chest )
- No finding when asthma is under control of under control
Investigation :
- Pulmonary function test -spirometry
- Estimate degree of obstruction
- >12% increase in FEV1, 15 minutes after B2 antagonist inhalation
- Chest x-ray hyperinflation,pneumothorax , emphysema
- Arterial blood gas analysis- hypoxia and hypocarbia
- Severe acute asthma -hypocarbia
- Skin hypersensitivity test
- Sputum examination
- Complete blood count eosinophils
- Elevated serum IgE level
Management of Bronchial Asthma:
Patients educations
- Avoidance of precipitating factor
- Avoid allergens
- Avoid pollutants
- Avoid drugs
Drug therapy
- Bronchodilator
- Beta2 antagonist
- Anticolingegcis
- Methylxanthines
- Antiinflammatory
- Corticosteroid, mast cell stabilizer, and leukotriene antagonist
- Inhaled corticosteroid
- Use of beta 2 agonists more than two times a week indicate the need for ICS
- Beclomethasone
- Budesonide
- Fluticasone
- Triamcinolone
- Leukotrienes antagonist
- Sodium cromoglycate
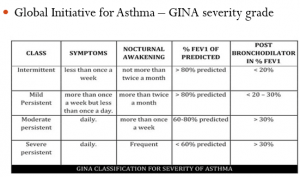
Classification of Bronchial Asthma
The severity of Bronchial Asthma can be classified according to the Global Initiative for Asthma – GINA severity grade as following:
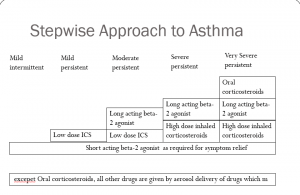
Stepwise Approach to Asthma:
We can do a stepwise approach to treat bronchial asthma as shown in the chart below.
Status asthmaticus:
- K/a severe acute asthma
- Severe airway obstructions
- Symptoms persist despite initial standard acute asthma therapy
- Severe dyspnea unproductive cough
- Patient updates upright position fixing shoulder griddle to assist accessory muscle of respiration
- Sweating control cyanosis tachycardia
Management of Status Asthmaticus:
- High concentration of oxygen through a facemask
- Ipratropium + salbutamol + NS in the ratio of 1:1:2 nebulized in the oxygen who don’t respond within 15-30 minute
- Inj. hydrocortisone 200 mg iv stat followed by 100 mg iv TDS
- Iv antibiotics -board spectrum
- monitor ABG
- Iv fluid – k supplementation may be required
- ET incubations and mechanical ventilation if the above treatment fails.
You might be interested to know about other Respiratory disorders.
Reference: WHO

Perfect balance of detail and simplicity. Very helpful read!
I all the time emailed this weblog post page to all my friends, since if
like to read it after that my links will too.
Grt but need many improvement dear