COPD (Chronic Obstructive Pulmonary Disease):
COPD (Chronic Obstructive Pulmonary Disease) is characterized by persistent airflow limitation that is usually progressive and associated with an enhanced chronic and inflammatory response in the airways and lungs to noxious particles and gases. It is a chronic slowly progressive disorder characterized by airflow obstruction which doesn’t change markedly over several months.
A common preventable disease of airways.
COPD includes (types):
- Chronic bronchitis
- Emphysema
Chronic bronchitis:
Chronic bronchitis productive cough for three months in each of two successive year in a patient in whom other causes of chronic cough have been excluded.
Any patient who coughed up sputum on most of the days at least three consecutive months for two successive year
Emphysema:
Abnormal and permanent dilatation of the air spaces distal to the terminal bronchioles that are accompanied by the destruction of the airspace walls without obvious fibrosis. Emphysema is a lungs condition that causes shortness of breath, the inflamed bronchial tubes produce a lot of mucus this lead to coughing and difficulty breathing is called emphysema.
Related Articles:
Tuberculosis | Causative Agent, Risk factor, Transmission, Symptoms and Treatment
Pneumonia Classification, Causes, Pathophysiology, Management and Prevention
Pathology:
- Airways
- Chronic inflammation
- increase numbers of goblet cell
- Mucous gland hyperplasia
- Fibrosis
- Narrowing and reduction in the number of small airways
- Airways collapse due to the loss of tethering causes alveolar wall destruction in emphysema
- Lungs parenchyma
- Emphysema affects the structure distal to the terminal bronchioles, consisting of the respiratory bronchiole, alveoli ducts alveolar sac, and alveoli know collectively as the acinus
Risk factors :
- Genetic
- Alpha1 antitrypsin deficiency is a genetic condition that is responsible for about 2%of cases of COPD. in this condition the body does not make cough of protein alpha1 antitrypsin
“Alpha1 antitrypsin protects the lungs from damage caused by protease and trypsin that are released as a result of the inflammatory response to tobacco smoke.”
Symptoms :
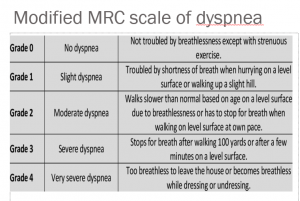
Characterized symptoms of COPD are chronic and progressive dyspnea cough and sputum production that is variable from day to day
- Dyspnea: progressive, persistent, and characteristically worse with exercise
- Chronic cough may be intermittent
- Sputum production: COPD patient commonly cough up sputum
- Other clinical features :
- Wheezing
- Chest tightness
- weight loss
- Respiratory infection
- Bounding pulse
- respiratory rate increase
- Restless
Physical sign:
- Inspection
- Barrel-shaped chest
- Use of accessory muscle of respiration
- Prolonged expiration during quiet breathing
- Expiration through pursed lips
- Paradoxical retraction of the lower interspace inspiration(hoover’s sign)
- Tripod position
- Palpation
- Decrease fremitus
- Percussion
- Hyper resonant
- Depressed diaphragm
- Diminution of an area of absolute cardiac dullness
- Auscultation
- Prolonged expiration
- Decreased breath sound
- Wheeze breath sound quiet breathing
- Crackle may be heard if the infection exists
Diagnosis of COPD:
Diagnosis of COPD is based on three facts
- Symptoms: Shortness of breath, chronic cough, sputum
- Exposure to risk factor: Smoking, occupation pollutants, indoor/outdoor pollutants
- Spirometry: Required to establish the diagnosis
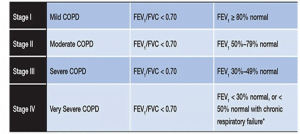
- Decrease FEV1/FVC (force vital capacity )ratio
- Increase total lung capacity (TLC)
- The presence of post-bronchodilator forced expiratory volume in one second (FEV1)<80%the predicated volume in combination with a FEV1 / forced vital capacity (FVC) <70% confirms the diagnosis of COPD
Assessment of severity:
Assessment severity of airflow limitation is done by gold criteria (Global inactive for chronic obstructive lungs disease )
Investigations:
- CBC, ESR: Findings seen only in exacerbation or acute infection
- Sputum analysis: helpful only in exacerbation or acute infection
- Chest X-ray:
- Tubular heart
- Hyperinflated lung field
- Low flat Diaphragm
- Emphysematous bulla
- Associated chest infection and complication
- Spirometry
- CT Scan
- Greater sensitivity and specificity for emphysema
- for evaluation of the bullous disorder
- ABG analysis:
- PaO2 < 8.0 KPa without PaCO2 > 6.7 KPa when breathing room air indicates respiratory failure.
Management:
- Based on principles of:
- Stop smoking
- Prevention of further process of disease
- Prevention and enhancement of Pulmonary functional capacity
- Avoidance of exacerbation and management of exacerbation to improve quality of life
- Stop Smoking
- Has the greatest capacity to influence the natural history of COPD
- Pharmacotherapy and nicotine replacement reliably increase long term smoking abstinence rate
- Bronchodilators
- central to the symptomatic management of COPD
- Improve emptying of lungs, Reduce dynamic hyperinflation and improve exercise performance
- Three major classes of Bronchodilators:
- Beta-agonists
- Short-acting: Salbutamol and Terbutaline
- Long-acting: Salmeterol and Folmeterol
- Anticholinergic agents: Ipratropium, Tiotropium
- Theophylline (a weak bronchodilator, which may have some anti-inflammatory properties)
- Beta-agonists
- Glucocorticoids:
- Regular treatment with inhaled glucocorticoids is appropriate for symptomatic patients with FEV < 50% predicted and repeated exacerbation.
- Chronic treatment with systematic corticoids should be avoided because of an unfavourable benefit to risk ratio.
- Combination therapy:
- Combination therapy of long-acting beta-agonists and inhaled corticoids show a significant additional effect in pulmonary function and a reduction in symptoms.
- Mainly in patient with FEV1 < 50% predicted.
- Management of exacerbation:
- Requires hospitalization
- Antibiotics- IV in acute exacerbation and oral after discharge
- Oxygen therapy
- Nebulization with Short-acting beta-agonists and anticholinergic agents.
- IV corticosteroids during hospitalization
- Requires hospitalization
- Others
- Mucolytic
- Antioxidant agents
- Oxygen therapy:
- Domiciliary oxygen therapy > 15 hrs/day
- Long term oxygen therapy (LTOT) improves survival, exercise, sleep and cognitive performance in patients with respiratory failure
- The therapeutic goal is to maintain SaO2 >90% and PaO2 > 60 mm of hg at sea level and rest
- Domiciliary oxygen therapy > 15 hrs/day
- Other treatment:
- Pulmonary rehabilitation
- Nutrition
- Surgery
- Bullectomy
- Lung volume reduction surgery
- Lung transplantation
Complications:
- Pneumothorax
- Cor pulmonale
- Exacerbation of COPD
- Respiratory Failure